- NHS teams are moving fast toward digital-first care, and custom apps are filling gaps that the standard NHS App cannot cover.
- Custom healthcare apps help reduce workload, cut waiting times, and improve how patients access care across Trusts and ICS regions.
- UK rules such as DTAC, NHS DSP Toolkit, NHS Login, and UK GDPR shape every stage of digital health development.
- Strong integration with EMIS, TPP, Cerner, and FHIR standards is key to making digital tools work smoothly inside NHS settings.
- A well-built custom app helps NHS organisations modernise pathways, support staff, and meet long-term digital goals without adding extra operational strain.
The NHS is undergoing a structural transition toward Digital-First Care, mandated by the Long Term Plan and the Federated Data Platform (FDP) rollout.
Trusts, ICSs, and primary care teams are all facing the same pressures: growing backlogs, limited staff capacity, and rising expectations from patients. Digital care pathways are no longer “future plans.” They are the foundation of how NHS organisations now deliver day-to-day care.
This is where custom healthcare app development in the UK plays a vital role. Off-the-shelf tools help, but they cannot handle the local needs of an NHS Trust, the workflow demands of clinical teams, or the integration work required across EMIS, TPP, Cerner, and shared care records. The push toward NHS app development is now tied directly to improving access, supporting staff, and keeping services running under real pressure.
Across the UK, leaders are prioritising solutions that improve patient flow, support virtual care, enable safer remote monitoring, and reduce the heavy admin load on clinicians. As a result, the demand for custom healthcare solutions in the UK is rising fast.
For NHS executives, the goal is simple: build digital tools that work, fit existing pathways, and meet UK rules such as DTAC, NHS DSP Toolkit, NHS Login, and UK GDPR. When done right, a healthcare mobile app in UK organisations can make care faster, easier, and more personal, without adding more strain to already-stretched teams.
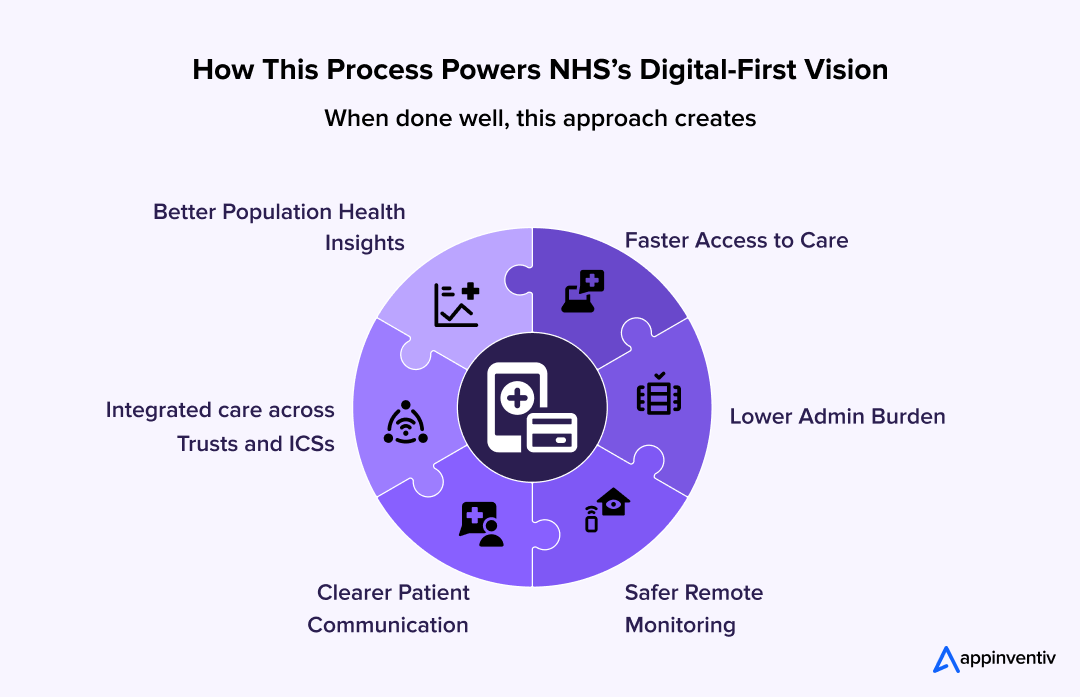
Custom systems are now helping the NHS move closer to its Digital-First Vision by supporting real patient needs, real clinical workflows, and the real challenges facing UK healthcare every day.
Digital Demand On The NHS App is Already Massive.
The NHS App saw 13.4 million unique logins in September 2025, showing how quickly patients are shifting to digital-first care.
Custom tools help Trusts extend this experience with local pathways, remote monitoring, and integrated workflows built for real NHS needs.
Why Building Custom Healthcare Apps for the NHS is a Strategic Opportunity
The NHS app development has reached a point where digital care is not optional. It has become the only practical way to keep up with rising patient needs, staff shortages, and long waiting lists. Trusts, ICSs, and primary care teams are now planning services around the NHS’s Digital-First vision, as the old way of working cannot support today’s demand.
Pressure on the NHS Is Higher Than Ever
Every organisation across the NHS is dealing with the same challenges:
- Outpatient waiting times at record levels
- GP practices are struggling to manage patient volumes
- Staff burnout due to high clinical and admin loads
- Complex systems that slow down daily tasks
- A growing need for safe remote care options
Digital tools such as virtual care NHS tech innovation pathways and simple patient-facing apps help ease this pressure. They reduce unnecessary appointments, cut manual work, and make it easier for patients to manage their own care.
Why the NHS App Alone Cannot Meet All Needs
The NHS App has improved access for millions. But it was never designed to meet the wide range of clinical and operational needs across all Trusts and ICSs.
Many UK organisations now rely on custom healthcare app development in the UK because:
- The NHS App follows a single, national design. Trusts cannot add their own pathways.
- Specialty care teams need deeper clinical features that the standard app does not support.
- Integrating EMIS, TPP, Cerner, PACS, and shared care records often requires custom work.
- Each Trust has its own workflows that cannot be changed to fit a fixed app.
This makes NHS app development a growing priority. Custom tools give organisations full control over the patient journey, staff workflows, and operational processes.
Why Trusts and ICSs Are Accelerating Custom Digital Builds
Across the UK, digital teams are now focusing on tools that support local needs. A generic platform cannot handle the care models of different regions, especially where community, acute, and mental health services work together.
NHS organisations are turning toward custom healthcare solutions in the UK, and teams can fully adapt because they offer:
- Localised care pathways designed for the area’s population
- Support for specialised services like maternity, oncology, respiratory, and urgent care
- Custom dashboards that give clinicians the data they need at the right time
- Better triage tools that help teams manage high-priority cases faster
With these tools, Trusts can design patient journeys that match their real workflows, not the other way around.
How Custom Healthcare App Development Powers Digital-First NHS Care
NHS’s Digital-First vision care works only when the tools fit real NHS workflows. That is why many Trusts and ICSs now choose custom healthcare mobile app development instead of using one-size-fits-all platforms.
These custom tools help teams modernise care, improve access, and support staff in a way that fits UK healthcare standards.
Below is a clear look at how this development process powers NHS’s digital-first vision care from the ground up.
Step 1: Set Clear Priorities for the Trust or ICS
Every NHS region has its own needs. Some want to improve outpatient flow, others focus on virtual wards, urgent care, remote monitoring, or better population health tools. The first step is agreeing on what matters the most:
This ensures NHS app development digital work supports real pressures, not just technology goals.
Step 2: Map Clinical Workflows With SME Support
A reliable NHS apps start with clinical input. Digital teams work with doctors, nurses, physios, and admin staff to map the exact steps of each pathway. This helps identify:
- Bottlenecks
- Safety risks
- Repetitive tasks
- Patient communication gaps
This mapping stage is also where Appinventiv’s teams run structured workshops, conduct clinical safety checks, and organise clear paths for each role involved.
Step 3: Engineering a “Cloud-First” & Interoperable Architecture
NHS app development systems require more than simple APIs; they require a robust data strategy. Our development focuses on:
- Data Standardisation: Using SNOMED CT for clinical terminology and DM+D for medicines to ensure data captured in-app is understood by EMIS and TPP SystmOne.
- Security & Hosting: Deployment on AWS London Region or Azure UK South to ensure 100% data residency compliance, protected by Cyber Essentials Plus standards.
- Interoperability: Implementation of HL7 FHIR (R4) resources to allow bi-directional data flow with the NHS Spine and Personal Demographics Service (PDS).
- Clinical Safety by Design: Every architectural decision is overseen by a nominated Clinical Safety Officer (CSO) to mitigate risks identified in the Hazard Log.
A stable foundation makes everyday work smoother for clinicians and reduces admin load.
This is also where integrated healthcare platforms that NHS teams rely on begin to take shape.
Step 4: Build UI/UX That Works for Every Patient
Digital inclusion is important for the NHS app development. Not all patients are confident with technology. To support everyone, the design follows NHS Digital patterns:
- Simple screens
- Plain language
- High contrast
- Clear icons
- Accessible layouts
This helps patients use the tool without stress and increases trust in digital pathways.
It also supports wider patient engagement apps that NHS patients use daily.
Step 5: Develop, Test, and Validate in NHS-Safe Conditions
Once the design and architecture are complete, development begins. During this stage, teams focus on:
- Clinical safety testing (DCB0129 / DCB0160)
- NHS Login sandbox integration
- EMIS and TPP sandbox testing
- Data protection checks
- Cybersecurity reviews
For NHS tech innovation, this is often the longest part of the journey because the systems must be safe, stable, and compliant.
Apps in this phase sometimes include AI healthcare apps UK organisations adopt for triage and admin support, but always with clinician oversight.
Step 6: Go-Live and Continuous Improvement
Once the app is stable and approved, the rollout begins. This includes:
- Pilots with small patient groups
- Staff training
- Real-time monitoring
- Weekly feedback loops
- Feature improvements
A digital-first NHS depends on continuous improvement. Trusts that update their tools regularly see better outcomes, fewer DNAs, and faster care.
This is also where long-term goals, such as digital health platform UK development and hospital app development UK strategies begin to grow across the wider system.
This is the real foundation behind the NHS’s digital-first vision and the key reason custom healthcare apps now play such an important role in daily care delivery.
Build Patient-Ready NHS Digital Pathways With Confidence
NHS organisations need tools that are fast, safe, and easy for patients and clinicians to use.
Our team designs healthcare mobile apps that support exactly what digital-first care requires.
What Custom Healthcare App Development Solves for NHS Trusts
NHS Trusts and ICSs are under constant pressure to deliver safe, fast, and consistent care. But most of the digital tools in place today were built years ago and cannot support the level of coordination modern care demands. This is why many UK organisations now invest in custom healthcare app development that fits their real clinical workflows and population needs.
Here’s what these solutions help NHS teams achieve.
Reducing Clinical and Admin Workload
Staff shortage is one of the biggest challenges across the NHS. Clinicians spend hours on tasks that can be automated or digitised. Custom tools help cut this load by offering:
- Digital forms that replace paper
- Automated triage for simple cases
- Asynchronous consultations for routine follow-ups
- Automated reminders and instructions for patients
This reduces pressure on GPs, nurses, and admin teams. It also helps them focus on patients who need in-person care the most. Many Trusts now use patient engagement apps NHS teams can rely on to keep communication simple and clear.
Improving Patient Access and Reducing Waiting Times
Long waits have become normal, but they don’t have to be. A well-built healthcare mobile app for UK patients can be used daily to help improve access through:
- Digital queueing
- Virtual-first triage
- Better scheduling tools
- Clear guidance before and after appointments
- Safer options for remote care
These features support the broader rise of virtual care NHS pathways and remote monitoring programmes. When patients can manage routine tasks on their own, clinical teams have more time to deal with complex cases.
Eliminating System Fragmentation
One of the biggest problems for NHS teams is dealing with multiple systems that do not work well together. Many Trusts still manage data across EMIS, SystmOne, Cerner, PACS, old portals, and paper documents.
This makes daily work slow and increases the risk of errors. Custom solutions allow organisations to build integrated healthcare platforms NHS teams can trust, where:
- Data flows smoothly across systems
- Clinicians don’t switch between screens
- Patient records stay consistent
- Tasks move faster across departments
Better integration also supports NHS tech innovation efforts aimed at modernising back-end systems.
Supporting ICS-Level Data Sharing
ICSs need a view of population health, not just single-Trust records. But this only works when data is standardised and shared safely. Custom digital tools help ICSs build:
- Shared dashboards
- Cross-Trust clinical views
- Standardised data models (FHIR)
- Integrated pathways linking primary, acute, and community care
This supports population health management apps in UK regions. They are now adopting to improve prevention, reduce hospital pressure, and support long-term condition management.
Any healthcare app built for the NHS must follow strict rules to keep patient data safe and clinical workflows reliable. These healthcare compliance standards are not optional; they form the core of every digital tool used across Trusts and ICSs. Meeting them early helps reduce project risks and makes the rollout path smoother.
DTAC (Digital Technology Assessment Criteria)
DTAC is the main check for all digital health tools in the NHS tech innovation. It covers:
- Clinical safety
- Data protection
- Cybersecurity
- Technical standards
- Usability and accessibility
A DTAC-ready app gives NHS teams confidence that the system is safe for daily patient use.
NHS DSP Toolkit
Any tool that handles NHS data must complete the DSP Toolkit. It confirms that the organisation has proper controls for:
- Data handling
- Access management
- Security processes
This helps Trusts ensure the partner they choose meets the NHS’s security expectations.
NHS Login, CIS2, and FHIR Standards
Most NHS apps require:
- NHS Login for secure patient access
- CIS2 for staff authentication
- FHIR for smooth data sharing with EMIS, TPP, Cerner, and other systems
These standards ensure the app fits into existing NHS workflows without adding extra work for clinicians.
UK GDPR and ICO Guidance
Patient data must be handled with care. Every app must follow UK GDPR rules, including:
- Clear consent
- Data minimisation
- Secure storage
- Proper retention policies
This protects both patients and NHS organisations from data risks.
MHRA Requirements (If the App Acts as a Medical Device)
If the app supports diagnosis, screening, or treatment, it may fall under MHRA rules. This requires:
- Clinical risk assessment
- Documentation
- Device classification
- Early checks help avoid delays later in the project.
Cyber Essentials Plus & ISO 27001
Beyond the DSP Toolkit, ensure the underlying infrastructure meets the gold standard for UK government cyber defense, providing an extra layer of indemnity for Senior Information Risk Owners (SIROs).
A compliant HealthTech app is easier for NHS teams to trust, safer to scale across regions, and more likely to support long-term digital-first care. Whenever teams choose custom healthcare app development, meeting these UK standards from day one is the safest way to ensure a smooth rollout.
Technical Note
Beyond the standard DSP Toolkit, custom builds should use Zero-Trust Architecture and OIDC (OpenID Connect) for NHS Login integration. This ensures that even in a multi-provider environment, patient identity and data integrity remain uncompromised at the edge.
Core Features of Custom Healthcare Apps for the NHS
NHS organisations need digital tools that support real clinical work, patient needs, and system-wide coordination. The features below represent what most Trusts and ICSs prioritise when building a custom digital health platform in the UK.
Patient Features
These features improve access and support safe self-management, especially for busy services:
- Simple symptom checkers
- Digital triage
- Appointment views and updates
- Medication and care reminders
- Secure patient–clinician messaging
- Remote monitoring tools for long-term conditions
Clinician Features
These features help staff work quickly and safely, without switching between multiple systems:
- Patient summaries linked to EMIS, TPP, or Cerner
- Structured forms that follow SNOMED CT
- Tools for virtual reviews and follow-ups
- Clear referral and task management
- Alerts for high-risk or priority cases
Operational and ICS Features
These features support efficient planning across services and regions:
- Real-time activity dashboards
- Demand and capacity tracking
- Flow insights for outpatient, community, and urgent care
- Shared care views for ICS teams
Real-World Use Cases Across the NHS Tech Innovation
Digital-first care is not a future goal; it is already happening across the NHS through practical, high-impact programmes. Below are real examples from UK Trusts and national NHS rollouts that show the key benefits of custom healthcare apps for the NHS.
Let’s see how custom healthcare app development is transforming day-to-day care.
Virtual Wards Across NHS England (200+ Virtual Wards Live)
NHS England’s national virtual ward programme supports patients with heart failure, COPD, frailty, and post-surgical recovery from home.
Patients use digital tools to record vitals, symptoms, and medication updates. Clinicians monitor dashboards and intervene early when readings change.
Impact reported for virtual care NHS England:
- Reduced avoidable admissions
- Faster discharge
- Improved patient confidence
- Lower hospital pressure during winter peaks
This is one of the strongest examples of how tools for remote patient monitoring that NHS teams rely on now support digital-first care.
eConsult and accuRx Transforming GP Triage and Access
Primary care uses digital triage widely across the UK. eConsult and accuRx are two of the most recognised custom-built solutions enabling:
- Digital-first consultations
- Structured symptom input
- Photo and document uploads
- Same-day routing to the right clinician
- Automated follow-ups and patient messages
These tools are used by over 3,000 GP practices, improving patient access and reducing admin time for staff. This is a clear, proven example of NHS app development improving first-contact care at scale.
Patient-Initiated Follow-Up (PIFU) Apps Used by Hospital Trusts
Dozens of hospitals across the UK—including University Hospitals Leicester, Royal Cornwall Hospitals, and Nottingham University Hospitals—are using PIFU pathways supported by mobile tools. Patients use apps or portals to:
- Report symptoms
- Request follow-ups
- Track their condition
- Receive personalised advice
This helps hospital app development in the UK and reduces unnecessary outpatient appointments, and focuses on patients who need specialist input.
MyChart & Patient Portals in UK Hospitals
Several NHS Trusts using Epic EHR also use its MyChart patient app — a powerful, real-world example of custom digital tools improving patient engagement. MyChart supports:
- Appointments
- Lab results
- Messaging
- Care plans
- Medication reminders
Trusts such as Guy’s and St Thomas’, Royal Devon, and Manchester University NHS Foundation Trust have reported better patient communication and reduced admin calls due to MyChart usage.
Talking Therapies (IAPT) Digital Pathways
NHS Talking Therapies providers use custom digital tools for:
- Online assessments
- Therapy session scheduling
- Progress tracking
- Self-guided CBT modules
- Safety plans and notes
Providers such as SilverCloud and Ieso are widely used across NHS regions and have published outcomes showing improved treatment access and reduced wait times.
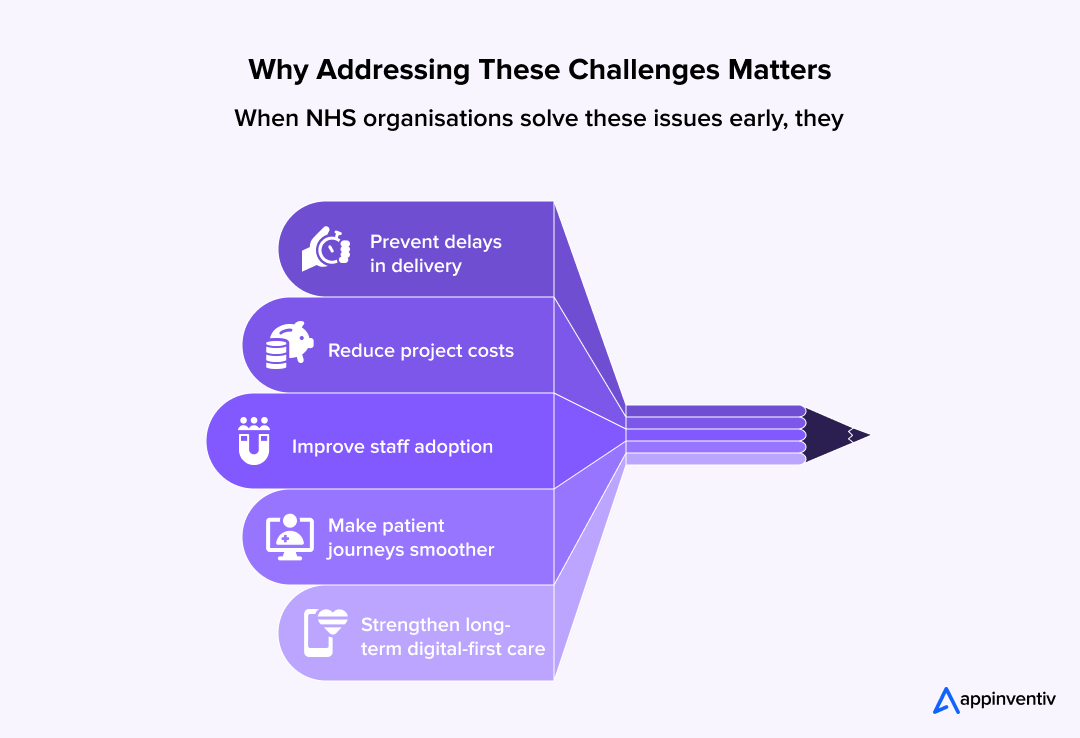
Challenges When Building and Scaling These Custom Healthcare Apps Within the NHS Context
Building digital tools for the NHS is not simple. Every Trust and ICS works differently, and every project must meet strict rules for safety and data protection.
Below are the most common challenges NHS teams face, along with how custom healthcare app development helps address them.
Challenge 1: Integrating With Complex and Legacy EHR Systems
Most Trusts use EMIS, TPP, or Cerner, often alongside older internal systems. These systems don’t always speak to each other. This slows down data flow and creates extra work for staff.
How custom apps solve it:
- Use FHIR standards for clean data sharing
- Build interoperability layers that link old and new systems
- Reduce screen-hopping for clinicians
- Keep patient data consistent across departments
This approach supports a smooth path to integrated healthcare platforms NHS teams increasingly need.
Challenge 2: Differences in Pathways Across Trusts and ICSs
Each region has its own protocols, patient priorities, and service models. A standard “one-size-fits-all” app rarely works.
Solution:
Modular, flexible designs that let teams:
- Add local pathways
- Tailor triage rules
- Adjust content and forms for their specialty
- Update features without starting again
This allows both Trusts and ICSs to build tools that fit their services, not the other way around.
Challenge 3: Clinical Safety Requirements and Compliance Risks
Another challenge when building and scaling these custom healthcare apps within the NHS context is that they must follow strict rules, like:
- DCB0129 (clinical risk for manufacturers)
- DCB0160 (clinical risk for Trusts)
- DTAC
- NHS DSP Toolkit
Meeting these rules takes time and clinical input.
Solution:
- Early involvement of clinical safety officers
- Clear documentation
- Risk assessment is built into each development stage
- Testing with real clinicians and patient groups
This ensures digital tools are safe for daily use.
Challenge 4: Digital Inclusion and Health Literacy Barriers
Not all patients are confident with technology. Some have limited digital skills, language barriers, or accessibility needs.
Solution:
Apps must follow NHS Digital guidelines:
- Simple language
- Clear layouts
- High contrast
- Multilingual support
- Offline-first options
- Easy onboarding steps
This helps more patients access care through digital paths.
Challenge 5: Cybersecurity and Data Protection Risks
NHS data is extremely sensitive. Security incidents can harm patients and disrupt care.
Solution:
- Zero-trust security models
- Encrypted communication
- Secure access through NHS Login or CIS2
- Audit trails for clinicians and admin users
- Alignment with NHS Secure Boundary guidelines
This gives Trusts confidence that patient data stays safe.
Cost and ROI of Custom Healthcare App Development for NHS Organisations
NHS teams plan digital programmes with tight budgets, clear outcomes, and strict compliance rules. Any move toward custom healthcare app development must give a clear picture of both cost and long-term value. Below is a simple, realistic overview based on UK market standards and the virtual care NHS project needs.
What Shapes the Cost of NHS-Grade App Development
The cost depends on how complex the project is and how deeply it must fit into existing NHS systems. Key factors include:
- Integrations with EMIS, TPP, Cerner, NHS Login, and Spine services
- DTAC, DSP Toolkit, and DCB0129/0160 requirements
- Depth of clinical workflows (e.g., virtual wards, outpatient triage, long-term condition support)
- Number of user roles (patients, clinicians, admin staff)
- Data dashboards and analytics
- Security controls such as encryption, audit trails, and access rules
- Scale across a Trust or ICS
Apps with deeper integrations and clinical workflows naturally cost more than simple patient-facing tools.
Typical Investment Range for NHS Organisations
High-level, safe, UK-aligned estimates:
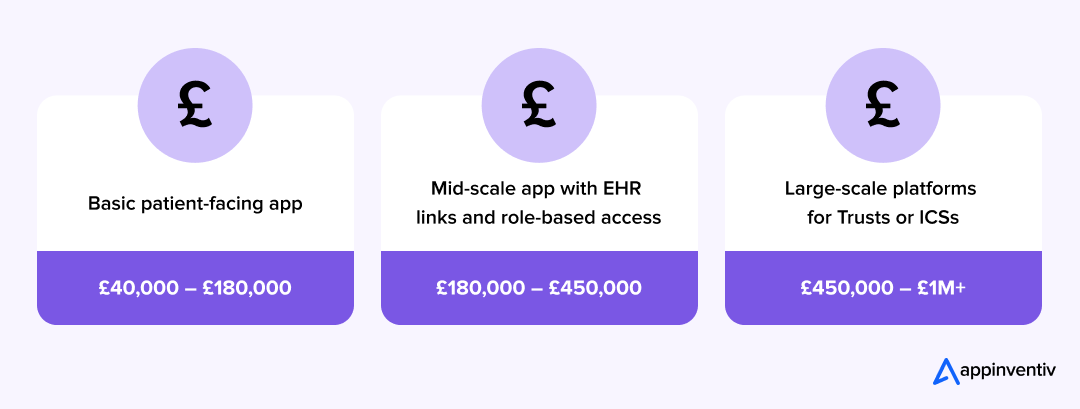
These ranges reflect development, testing, compliance checks, and integration work.
Ongoing Costs to Expect
Custom NHS tools need regular updates to stay safe and compliant:
- DTAC updates
- Cybersecurity patches
- Feature expansion
- API changes from EMIS, TPP, or NHS Login
- Growing user volumes across Trusts or ICSs
NHS teams usually treat this as an annual operational cost, not a one-time spend.
Also Read: How Much Does It Cost to Build a Healthcare App?
Measuring ROI: Beyond Digital Transformation
For NHS Trust Boards, the business case for custom apps must demonstrate both Qualitative Outcomes and Cash-Releasing Benefits.
| Metric Category | Impact of Custom Digital Pathways |
|---|---|
| Operational Efficiency | 30% reduction in “Did Not Attend” (DNA) rates via automated PIFU (Patient-Initiated Follow-Up) triggers. |
| Clinical Productivity | Saving ~2.5 hours per shift for clinicians by automating observations via Remote Patient Monitoring (RPM). |
| Cash-Releasing | Lowering the cost-per-contact by shifting routine follow-ups to asynchronous digital channels. |
| System Flow | Accelerated “Medically Fit for Discharge” (MFFD) timelines through Virtual Ward monitoring. |
The biggest ROI comes from improved flow. When patients self-manage simple tasks, staff can focus on the cases that truly need clinical attention.
Why This Matters for Digital-First NHS Care
A well-built digital tool:
- Cuts operational strain
- Improves patient access
- Supports safer remote care
- Reduces dependency on fragmented systems
- Helps Trusts meet digital targets faster
This is why many NHS organisations see custom digital tools not as a cost, but as a long-term operational asset.
Emerging Trends Shaping Digital-First NHS Care
The NHS is entering a phase where digital tools will shape most routine care. The next few years will be defined by solutions that reduce pressure on staff, support safer remote care, and help Trusts work as one system. Below are the trends that will guide this shift.
AI-Supported Triage and Care Routing
AI-supported triage tools are becoming more common in urgent care, GP access, and outpatient pathways. They help teams sort cases faster, highlight risk, and direct patients to the right support without long waits. The rise of AI in healthcare apps in the UK that are being tested today will soon play a bigger role in frontline decision-making.
Remote Monitoring Through Wearables and Home Devices
Virtual wards and home-based monitoring will expand. Patients with long-term conditions will track vitals using simple devices and share outcomes through integrated apps. This reduces avoidable admissions and gives clinicians early signals when a patient’s condition changes.
More Personalised and Self-Directed Care Pathways
Digital tools will help patients manage more of their care on their own. Apps will guide people through treatment plans, rehabilitation tasks, and symptom tracking with clear steps. This supports the NHS goal of helping patients stay well at home and reduces the demand on clinics.
Stronger ICS-Wide Data Sharing and Shared Care Records
Integrated Care Systems need a whole-population view. The next stage of NHS digital transformation will strengthen shared care records, so staff across primary, acute, mental health, and community teams see the same information. This will support better planning, smoother handovers, and more accurate population health insights.
Automation for Admin and Routine Clinical Tasks
Simple tasks such as appointment reminders, repeat requests, basic patient queries, and pathway updates will shift to automated assistants. These tools will help free up staff time and keep clinics running smoothly. Many Trusts already use messaging tools for routine tasks, but wider adoption will follow.
Predictive Insights for Capacity and Demand Management
NHS teams are moving toward data-driven planning. Predictive insights will help Trusts manage beds, clinics, rotas, and high-demand periods more effectively. This will help services stay stable even when patient volume rises.
| Digital-first care is becoming the default model. Organisations that invest early in flexible, well-structured digital tools will adapt faster, reduce operational strain, and stay aligned with national NHS goals.
This also strengthens the case for custom healthcare app development, as Trusts increasingly need systems built for their local pathways, regional priorities, and ICS-level coordination. |
Why NHS Organisations Can Trust Appinventiv as a Digital-First Partner
Appinventiv offers custom healthcare mobile app development services. NHS teams need partners who understand clinical workflows, strict compliance rules, and the scale at which UK healthcare operates. Appinventiv’s work in regulated healthcare environments puts us in a strong position to support Trusts and ICSs moving toward custom digital solutions.
Clinical-Grade Engineering at Scale
Appinventiv has a team of 1,600+ engineers, including 300+ healthcare specialists who work on digital solutions built for high-volume patient care.
These teams understand how clinical systems work, how data flows across departments, and what clinicians need in day-to-day practice.
We offer custom mobile app development in the UK and have already delivered 3,000+ digital products. Many of them are in regulated environments where safety, stability, and uptime are critical.
Deep Experience in Healthcare Platforms
Our teams have built large-scale digital health platforms with:
- Remote monitoring features
- Patient communication tools
- Clinical dashboards
- Care management systems
- Secure data exchange
- Multi-role access controls
These builds mirror the needs of NHS pathways such as virtual wards, PIFU models, outpatient transformation, and long-term condition support.
Strong Foundations in Security and Compliance
Appinventiv works with global healthcare organisations that follow strict compliance standards. This includes:
- HIPAA-aligned engineering practices
- ISO 27001-certified security processes
- Encrypted data handling
- Secure identity frameworks
- Detailed audit trails
These capabilities align well with UK requirements, such as:
- DTAC
- NHS DSP Toolkit expectations
- DCB0129 and DCB0160
- NHS Login and CIS2 integration models
- FHIR-based data exchange
Our teams can adapt these frameworks to meet NHS-specific needs.
Integration Capabilities for NHS Environments
We understand that NHS systems need seamless integration rather than additional complexity. Our engineering teams have strong experience in:
- FHIR-based APIs
- Large EHR integrations
- Secure authentication flows
- Scalable cloud deployments
This experience supports the integration needs of EMIS, TPP, Cerner, and shared care record environments, the systems at the heart of NHS digital operations.
Proven Delivery for High-Stakes, High-Scale Projects
Appinventiv has built systems used by millions of users across the world. This includes:
- Country-wide digital health deployments
- High-traffic patient platforms
- Enterprise-scale care management systems
- AI-supported clinical workflows
These projects required stability, continuous availability, and the ability to manage large patient populations, the same conditions NHS Trusts operate within every day.
NHS teams need partners who understand the pressure of large healthcare systems, the pace of digital change, and the responsibility that comes with handling clinical workflows.
Appinventiv brings engineering scale, healthcare experience, regulatory understanding, and system integration strength. This makes us a reliable choice for Trusts and ICSs seeking custom tools that support digital-first NHS care.
Ready to Build Your NHS-Aligned Digital Solution?
If your Trust or ICS is planning new digital pathways, our healthcare engineering teams can support every stage, from design to deployment.
Conclusion: Moving the NHS Toward a Digital-First Future
The NHS app development is moving toward a future where digital tools support most parts of care. Custom healthcare apps now play a central role in this shift. They reduce pressure on staff, improve access for patients, and help Trusts and ICSs work as one system. They also fill the gaps that standard platforms cannot address, especially when local pathways or advanced integrations are required.
For NHS leaders, the goal is clear: build digital solutions that are safe, compliant, and able to scale across services. To achieve Digital-First NHS Care, Trusts must move beyond siloed tools. The priority for 2026 is creating integrated healthcare platforms that are DTAC-compliant, FHIR-enabled, and clinically safe. Custom healthcare app development in the UK provides the flexibility to map local pathways (like Maternity or Oncology) into a unified digital interface that reduces the total cost of care.
This is where a strong development partner matters. With deep healthcare experience, reliable engineering practices, and proven delivery at scale, Appinventiv supports organisations aiming to build tools that fit real clinical and operational needs. Connect with Appinventiv to build the right solution.
Frequently Asked Questions
Q. How Are Custom Healthcare Apps Enhancing Patient Care in the NHS?
A. Custom healthcare apps improve patient care by offering easy access to services, better communication with clinicians, and remote monitoring. These tools allow patients to manage their own care, reduce waiting times, and receive more personalised treatment. By supporting features like digital triage and remote consultations, custom apps help ensure patients get the right care, at the right time, without unnecessary hospital visits.
Q. What Role Does Integration with NHS Systems Play in App Development?
A. Integration with NHS systems, like EMIS, TPP, and Cerner, ensures that custom healthcare apps work smoothly within existing workflows. It allows patient data to flow securely between systems, reducing errors and saving time. Integration with systems like NHS Login and shared care records also enables seamless access for both patients and clinicians, ensuring a more coordinated care experience across Trusts and ICSs.
Q. How Do Custom Apps Improve Operational Efficiency in NHS Facilities?
A. Custom apps reduce the time spent on administrative tasks and improve workflow efficiency. They automate tasks like appointment scheduling, patient check-ins, and follow-ups. Clinicians can access real-time data, reducing delays and improving decision-making. This allows staff to focus more on patient care and less on time-consuming processes, ultimately lowering costs and improving service delivery across NHS facilities.
Q. What Are the Key Benefits of Digital-First Care Models Enabled by Custom Apps?
A. Digital-first care models allow NHS organisations to provide faster, more accessible care. Custom apps enable remote consultations, virtual wards, and digital triage, all of which reduce the strain on in-person appointments. Patients can access services anytime, anywhere, improving convenience and satisfaction. This also frees up valuable resources, allowing clinicians to focus on patients who need in-person care, ultimately improving care quality and operational efficiency.
Q. How Can NHS Trusts Measure Success and ROI of Custom App Implementations?
A. NHS Trusts can measure success through key performance indicators (KPIs) such as reduced waiting times, improved patient satisfaction, and enhanced clinician productivity. ROI can be tracked by looking at operational savings, such as reduced administrative costs, fewer missed appointments, and reduced hospital admissions. Monitoring the time savings for clinicians and the improved access to care for patients provides a clear picture of how a custom app contributes to long-term value.
Q. What Are the Future Trends in NHS Healthcare App Development?
A. The future of NHS healthcare app development will focus on AI-driven tools for triage and clinical decision support, enhancing remote monitoring through wearables, and expanding virtual care pathways. Integration with predictive analytics will help forecast demand and improve capacity management. Patient-centric apps will evolve to support more self-managed care and personalised treatment, giving patients greater control and making the NHS more efficient overall.