Key Takeaways
- Streamlined Operations: Patient waitlist management system integrates scheduling, billing, and patient data into a unified platform, enhancing hospital efficiency and patient care.
- Real-World Customization: Development involves understanding real workflows and incorporating feedback to ensure system adoption.
- Cost Efficiency: The cost of developing Patient Waitlist Management Software ranges from $40K to $400K, depending on the system’s scale and complexity, with costs increasing based on features like AI, EHR integration, and compliance.
- Compliance and Security: Patient waitlist management software must comply with HIPAA/GDPR, ensuring robust security and data protection.
- Scalable & Customizable Solutions: Whether you’re scaling to multiple locations or adding new features like Patient scheduling and waitlist systems, a flexible PWMS allows for future growth without costly overhauls.
Healthcare facilities constantly face scheduling challenges and patient flow issues. Patient waitlist management software development can fix these issues by organising waitlists, setting priorities, and notifying patients when appointments become available. The software helps providers fill empty slots, manage patient volume more effectively, and avoid wasting scheduling time.
Patient Waitlist Management Software development differs from complete Patient Management Systems (PMS). Full PMS platforms handle everything: EHRs, billing, telemedicine, patient histories, and insurance verification. Lots of complexity there. Waitlist software solves one problem: efficiently filling open slots. It’s not running your whole practice. It handles scheduling, quickly filling cancellations, prioritizing urgent patients, and keeping calendars full, rather than having providers sit around with nothing scheduled.
Hospitals implement waitlist software for specific operational reasons: patient flow gets unbalanced, appointment gaps waste resources, and scheduling problems frustrate staff and patients.
The global digital health market hit USD 427.24 billion in 2025. Fortune Business Insights expects the market to reach USD 1,500.69 billion by 2032. That’s 19.66% growth annually. Deloitte’s 2025 Global Health Care Outlook reports that health system leaders are prioritizing digital transformation. Why? Operational efficiency. Productivity improvements. Better patient engagement. These outcomes directly affect care quality and financial results.
This guide explains how to build effective waitlist systems, the development process, features that work, realistic costs, and how they connect to improvements in patient experience.
Stay Ahead with Smart Scheduling
As the digital health market surges to USD 1,500.69 billion by 2032, the time to innovate is now. Partner with us to build a dynamic Patient Waitlist Management System.
Key Considerations for Developing an Effective Patient Waitlist Management System
Building a Patient Waitlist Management System that works seamlessly in practice goes beyond just ticking off technical specifications. It’s about creating a solution that healthcare teams will use multiple times every day, under pressure, when they’re tired, and always when accuracy is critical.
For many healthcare providers, this means aligning the Patient Waitlist Management System goals with broader software development lifecycle objectives, ensuring that everything from scheduling and queuing to follow-ups is part of a unified digital infrastructure.
Start with Real People and Real Problems
Every stakeholder group walks into your clinic with different needs. Patients want to book appointments without endless calls and understand their bills. Administrative staff need billing and scheduling that actually makes sense.
If your Patient Waitlist Management software forces people to change their work instead of supporting their current methods, adoption will be a constant battle. Talk to each group early. Watch them work. Find out what slows them down. When the system feels like it was built for their workflow, they’ll use it. When it doesn’t, they’ll find workarounds, and your software risks becoming shelfware.
Map out what each stakeholder needs and what frustrates them. Talk to frontline staff, doctors, nurses, and administrators. Understand their daily routines. The more your software aligns with existing tasks, the easier the implementation becomes.
That’s why many healthcare providers develop Waitlist management systems for hospitals to capture real-world challenges and design flows that feel natural for each role.
Build Compliance In
Healthcare data isn’t just another dataset — it represents people’s most sensitive medical information. That’s why strict regulations like HIPAA in the U.S., GDPR in Europe, and similar global laws exist. They’re not suggestions or checkboxes; they’re essential safeguards designed to protect patient privacy and trust.
Your Patient Waitlist Management software needs encrypted storage, secure data transmission, and detailed audit trails. Role-based permissions should ensure staff only see what they need to. The time to think about compliance is before you write your first line of code, not after development ends.
And it’s not just about avoiding penalties. One data breach can destroy years of patient trust. That’s why modern projects consider HIPAA compliance in waitlist software an inseparable part of building healthcare platforms.
Design for Scalability
Too many healthcare organizations build for their current state and struggle when things shift. Patient volume grows, rules evolve, and telemedicine becomes the norm.
The smart move? Build flexibility in. Your system should support new modules, analytics, remote monitoring, and AI features — without tearing everything down. This adaptability matters even more if you plan to create Patient waitlist management software for hospitals in the future.
Integration Isn’t Optional- It’s Central
Your Patient Waitlist Management software must work within a larger tech ecosystem —Electronic Health Records, billing platforms, pharmacy systems, and more. If they don’t connect, staff waste hours manually transferring data, increasing the risk of errors.
Plan integrations early. Use standards like FHIR and HL7 that the rest of healthcare already follows. When information moves seamlessly, your staff can focus on patients, not paperwork.
For example, Digital Waitlist Management Software development efforts ensure that scheduling data remains unified and avoids double-booking or missing records — two common challenges in patient scheduling systems.
Also Read: Medical Scheduling Software Development Cost Estimation
Optimize Usability for Rapid Adoption
Spend a day in any clinic and you’ll understand why design matters. Staff deal with dozens of patients, calls, and emergencies daily. They need intuitive software, not one that requires a manual to schedule an appointment.
Clear dashboards, predictable navigation, and mobile access for doctors on the move all make a difference. The easier the tool, the faster teams adapt. This simplicity also extends to the key features of patient waitlist system design, where intuitive displays and clear next steps dramatically reduce training time.
Implement Multi-Layered Security to Safeguard Trust
Because it does, healthcare breaches are headline-making and expensive. Encrypt everything- data at rest and in transit. Use multi-factor authentication, role-based access, and ongoing security monitoring. Security audits and compliance checks are part of your foundation, not afterthoughts. Patients notice when their data is treated seriously.
When planning companion systems, such as Patient waiting list management system modules, the same controls and HIPAA compliance principles should be applied from the beginning.
Turn Data into Decisions, Not Just Reports
Every appointment, test, and follow-up generates information. The challenge is using it well. Real-time analytics can show patterns- like which slots fill fastest, which departments face bottlenecks, or which patients frequently cancel.
These insights help you plan staffing, reduce wait times, and improve care. In fact, data-driven insights often highlight the benefits of Waitlist management software —especially when tracking how effective the waitlist is at reducing no-shows and increasing appointment utilization.
How to Build a Patient Waitlist Management System?
You don’t start a Patient Waitlist Management System project by picking tech stacks or writing user stories. You start by figuring out how people actually work, not how they say they work. The best systems come from observing the real, sometimes messy, routines of hospitals and clinics.
It requires a comprehensive understanding of real healthcare workflows and a detailed development approach. Here’s how you can build a robust PWMS:
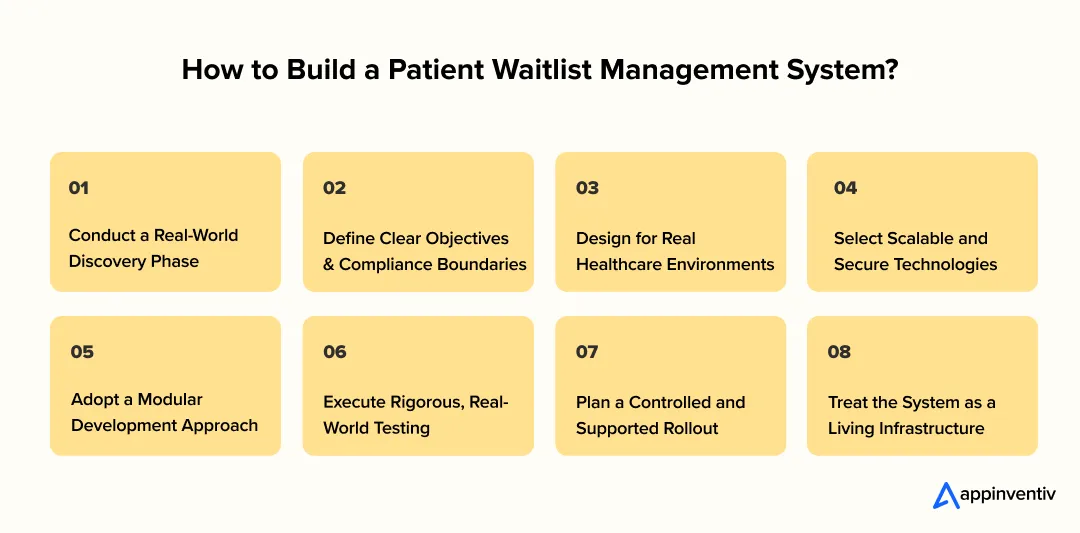
1. Conduct a Real-World Discovery Phase
Before asking your team to write a single line of code, spend time with your people. Talk to doctors juggling 10 patients an hour, nurses updating records between calls, and admin staff hunting for missing files —even a few patients, if possible. You’ll see patterns everywhere: duplicate data entry, double bookings, and follow-ups that depend on someone remembering an email.
These cracks are exactly where your Waitlist Management software should deliver value. The goal isn’t to map an “ideal” process but to understand what really happens when things get hectic.
Many teams at this stage also develop Waitlist management systems for hospitals to capture real workflow gaps and determine how a Patient scheduling and waitlist system could reduce waiting times or balance load between departments.
2. Define Clear Objectives and Compliance Boundaries
Once you’ve seen how things operate, set your goals clearly. Ask: What specific problems should this system fix? What’s worth automating, and what still needs a human touch?
At the same time, anchor everything in data privacy. Regulations such as GDPR, HIPAA, and local healthcare laws form the foundation. If you design without security first, you’ll pay for it later- both financially and reputationally.
3. Design for Real Healthcare Environments
Healthcare software isn’t used in quiet offices. It’s used during 12-hour shifts, in noisy wards, often when someone’s health depends on it. Start small- build a prototype, give it to real users, watch how they interact. Notice hesitation points or repetitive steps, fix them, and test again. Catching friction early saves weeks later and improves usability.
The same approach helps define the features of patient waitlist system design- clarity, minimal clicks, and clear status updates for both staff and patients.
4. Select Scalable and Secure Technologies
Your technology choices decide how well your system performs years from now. Use proven frameworks such as Node.js, Spring Boot, or .NET Core for back-end work; React or Angular for front-end interfaces.
Opt for the best databases, such as PostgreSQL or MongoDB, and plan integrations early —especially with billing systems, EHRs, and telehealth apps.
Scalability becomes even more important when you build a Patient waitlist management system for hospitals across multiple branches, or when you merge it into an existing Patient waiting list management system. A cloud-ready architecture futureproofs your setup and simplifies maintenance later on.
5. Adopt a Modular Development Approach
Avoid trying to build everything at once. Break your waitlist management software into clear modules—appointments, billing, patient data, and analytics—and develop each one incrementally. Test, refine, and move to the next.
This modular strategy ensures that if one feature needs rework, the rest stays stable. It’s the same logic used in developing a custom hospital waitlist system: hospitals begin with appointment handling, then add queue visibility, and later add analytics dashboards. Incremental growth reduces risks and shortens time to value.
6. Execute Rigorous, Real-World Testing
Testing in healthcare isn’t optional; it’s proof that your system can withstand real pressure.
Simulate peak loads, multiple logins, overlapping telemedicine sessions, and concurrent data entries.
Test encryption, access controls, and audit trails just as you’d test usability. A security gap or crash at scale isn’t just a technical issue; it’s a patient safety issue.
Healthcare leaders also test the performance of the patient scheduling and waitlist system under heavy demand to see how well it integrates with the virtual queuing system during peak hours.
7. Plan a Controlled and Supported Rollout
Never flip the switch for your entire hospital at once. Start with one department or floor, gather feedback, fix issues, and expand gradually.
When training staff, show them how the patient waitlist management software makes their day easier, not through slides, but through real examples. Once they see the time savings, adoption follows naturally.
Pilot programs often include early testing of building Healthcare queue management software, where staff and patients test new check-in or callback flows before system-wide deployment.
8. Treat the System as a Living Infrastructure
A patient waitlist management software is never truly “done.” It’s a living system that evolves with your hospital. Regulations shift, APIs change, and users find new pain points. Schedule updates, run quarterly audits, and keep monitoring security performance.
Organizations that view their waitlist management software as dynamic, rather than static, end up with systems that age gracefully.
Many of them continue to develop a Waitlist management system for hospitals as new branches open or new departments form, aligning their software development roadmap with operational growth.
Also Read: Hospital Management System Software Development
Stay Ahead with Smart Scheduling
As the digital health market surges to USD 1,500.69 billion by 2032, the time to innovate is now. Partner with us to build a dynamic Patient Waitlist Management System.
Tech Stack for Patient Waitlist Management Software Development
A good Patient Waitlist Management System is built step by step. The technology stack determines how easy the system is to use, how securely it stores data, and how well it scales as patient numbers and hospital branches grow.
This foundation also supports the development of Healthcare queue management software and the extension of Patient waiting list management system capabilities for multi-location operations.
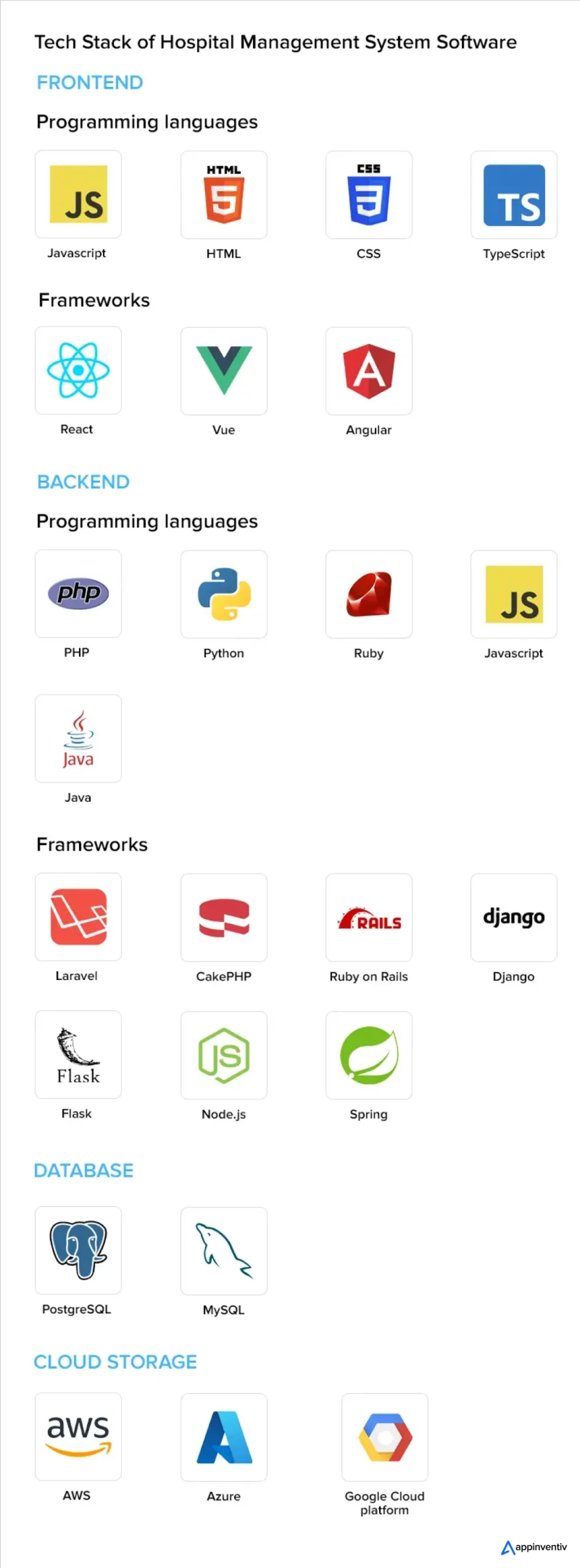
1. Frontend
This is what doctors, nurses, administrative staff, and patients see and use daily. It should be clean, quick, and intuitive.
React or Angular is ideal for responsive dashboards and patient portals —React offers flexibility, while Angular provides built-in structure.
- Flutter or React Native enables a single mobile app to run on both iOS and Android, keeping development costs manageable.
- HTML5, CSS3, and JavaScript ensure smooth, device-friendly web experiences.
Strong, responsive interfaces become even more valuable when integrated with Digital Waitlist Management Software development modules that display live wait times and appointment queues.
2. Backend
This is where real processing happens: moving data, managing logic, and keeping everything secure.
- Node.js / Express.js – great for real-time updates such as appointment notifications or telehealth calls.
- Java / Spring Boot – trusted for enterprise hospital systems that need long-term reliability.
- Python / Django – ideal if you plan to include AI or analytics.
- .NET Core – perfect for high-security healthcare setups.
Robust backend planning also supports custom hospital waitlist system development, where queue logic, patient notifications, and clinic-specific business rules are handled behind the scenes.
3. Database
Choose a database that can manage large volumes of confidential information and maintain integrity as the system scales.
- MySQL, PostgreSQL, or Microsoft SQL Server – solid for appointments and billing data.
- MongoDB or Couchbase – ideal for unstructured information such as imaging or wearable feeds.
- Redis – boosts real-time speed for alerts and reminders.
For hospitals investing in patient waitlist management software development, well-structured databases are critical for efficiently tracking queue positions, cancellations, and callback times.
4. Cloud and DevOps
Downtime in healthcare simply isn’t acceptable. AWS, Azure, or Google Cloud deliver HIPAA-ready infrastructure that scales on demand.
Docker and Kubernetes containerize different services safely, while CI/CD tools such as Jenkins or GitLab push updates without interrupting care.
Cloud-based architecture is now central to Digital Waitlist Management Software development, allowing clinics to coordinate patient flow across multiple locations in real time.
5. Integrations
Your patient waitlist management software should talk to existing systems. FHIR and HL7 standards enable patient data to flow smoothly between EHRs, labs, and billing systems.
Payment and insurance APIs simplify transactions, while telemedicine SDKs (Zoom, Twilio, Agora) enable secure virtual visits.
These integration points also help connect the Patient scheduling and waitlist system data with billing, alerts, and reporting features, preventing duplicate entries and manual rework.
6. Security and Compliance
Patients entrust you with their most private details. Protecting that trust is non-negotiable. Encrypt all data (TLS/SSL in transit, AES-256 at rest). Use role-based access so only authorized staff can view records. Implement continuous monitoring using tools such as the ELK Stack or Splunk, and conduct regular vulnerability scans with OWASP ZAP or Fortify.
These same principles must govern HIPAA compliance in waitlist software as well—especially when the waitlist module handles SMS reminders or live patient status updates within a Patient waiting list management system.
7. Analytics and Reporting
Every interaction adds to your hospital’s data stream. Turning that into insight drives smarter decisions.
- Power BI, Tableau, and Looker create user-friendly dashboards for staff and executives.
- Python or R can predict patient flow or appointment trends
- Apache Spark or Hadoop handles large imaging or device datasets.
Analytics also surface the features of patient waitlist system performance, such as average waiting times, filled cancellations, and queue efficiency, helping leadership measure progress and refine policies.
Also Read: Medical Practice Management Software Development
Must-Have Features of Patient Waitlist Management System
Good patient waitlist management software should make everyone’s job easier, doctors, nurses, front-desk teams, and administrators. It must keep information secure, automate repetitive work, and make every patient interaction smoother.
In many facilities, these same principles guide patient waitlist management to ensure that scheduling and access stay balanced.
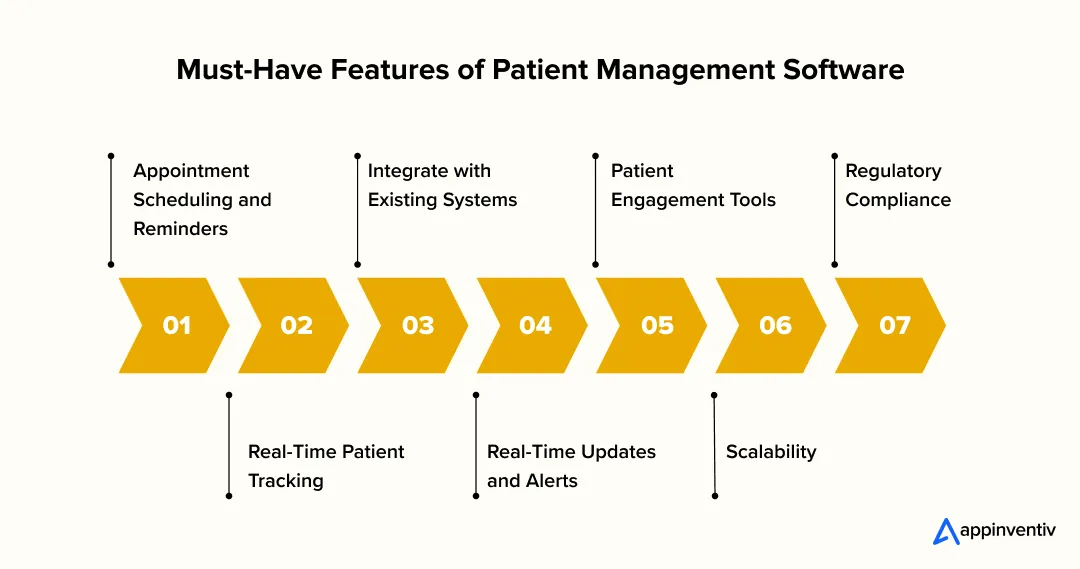 1. Appointment Scheduling and Reminders
1. Appointment Scheduling and Reminders
Missed appointments cost both time and revenue. A smart patient waitlist management software allows patients to book, reschedule, or cancel easily, with instant confirmations by SMS or email. Combining this with patient waitlist management tools helps clinics automatically fill cancellations and reduce idle time. Some advanced setups also use virtual queuing systems to efficiently manage walk-ins.
2. Real-Time Patient Tracking
Track patient status, appointment history, and wait times in real time, allowing staff to prioritize urgent cases and quickly update patients. This feature streamlines workflows, reduces bottlenecks, and ensures better resource utilization, leading to a smoother, faster patient experience.
3. Integrate with Existing Systems
The waitlist management system must integrate seamlessly with existing healthcare technologies, such as EHR (Electronic Health Records), billing systems, and telemedicine solutions. This ensures that patient data flows smoothly across platforms, reducing the chances of errors and duplicative work.
4. Real-Time Updates and Alerts
When someone cancels or misses an appointment, patients waiting for earlier slots should know immediately. Real-time alerts let people on the waitlist grab open spots fast. This fills schedule gaps that would otherwise waste provider time and delay care for patients stuck waiting.
5. Patient Engagement Tools
Mobile apps for communication and notifications keep patients informed without constant phone calls. People want to know where they stand on the waitlist and when they might actually get seen. Regular updates reduce the frustration of waiting in the dark and wondering if they’ve been forgotten.
6. Scalability
As healthcare facilities grow, the system must be scalable. Whether it’s adding new departments, clinics, or locations, the system should support easy expansion without significant redesigns or downtime.
7. Regulatory Compliance
Patient trust depends on transparency and security. Whether operating under HIPAA, GDPR, or regional frameworks, compliance isn’t optional. Ensure all data access is logged, encrypted, and limited by role. This discipline naturally extends to HIPAA compliance for the system, where patient reminders, queue alerts, and communication logs must follow the same privacy principles.
Also Read: An Entrepreneur’s Guide to Patient Engagement Software
Patient Waitlist Management Software Development Cost
When you decide to develop a Waitlist Management System for hospitals, you’re not just budgeting for software- you’re shaping how your team works every single day. How quickly can they pull up a record? How easily can a patient book an appointment? How confidently can you say, “Yes, their data is safe.”
That’s what this investment really covers. So before you dive in, it’s essential to understand what drives the cost- and how add-ons like patient waitlist management software development can affect both budget and scalability.
- Core Functionality Affects Cost: The cost depends on the features you need. A basic system is affordable, but adding advanced features like telemedicine or multi-branch support will raise the price. While initial costs may be higher, they lead to better service and faster patient handling.
- Tech and Hosting Choices Impact Budget: Cloud services like AWS offer scalability but come with recurring costs. Running servers in-house gives more control but costs more upfront. Adding integrations and compliance checks also adds to the price.
- Design Drives User Adoption and ROI: A simple, easy-to-use design keeps users happy and improves workflow. If the interface is frustrating, no matter how powerful the system, users won’t stick around.
- Team Location and Composition Matter: Development costs vary by team location. A U.S.-based team may cost more than one in Southeast Asia. The team size and expertise also play a role in how much it’ll cost.
- Maintenance Adds Long-Term Value: Once your system is live, you’ll still need to budget for updates, security patches, and adjustments as your hospital grows or regulations change.
- Start Simple, Then Scale: Start with the basics—like scheduling and patient records—and add features as you go. This keeps your budget in check and allows for smoother scaling as your needs grow.
The cost to build a Patient Waitlist Management Software typically ranges from $40,000 to $400,000, depending on scale and complexity.
| Project Type | Includes | Estimated Cost (USD) |
|---|---|---|
| MVP | Core modules like scheduling and billing. | $40K – $80K |
| Mid-Level | Adds mobile apps, integrations, and automation. | $80K – $200K |
| Enterprise | Includes AI, IoT, EHR integration, and compliance. | $200K – $400K+ |
Here’s a cost breakdown of patient waitlist management software phase-wise:
| Component | Features | Estimated Range (USD) |
|---|---|---|
| Discovery & Research | Workshops, stakeholder interviews, workflow mapping, compliance (HIPAA/GDPR) planning | $10,000 – $35,000 |
| UI/UX Design | Wireframes, interactive prototypes, user testing, accessibility optimization | $12,000 – $40,000 |
| Backend & API Development | Core modules (patients, scheduling, billing), integrations with EHRs/labs, and authentication | $60,000 – $180,000 |
| Frontend / Mobile Apps | Web dashboard + iOS/Android apps, responsive design, real-time sync | $25,000 – $90,000 |
| Integrations | Insurance systems, diagnostic APIs, payment gateways, and telehealth modules | $15,000 – $60,000 |
| Testing & Quality Assurance | Functional, performance, and security testing, compliance validation | $8,000 – $35,000 |
| Infrastructure & Hosting | Cloud setup (AWS/Azure/GCP), CI/CD pipelines, server monitoring, backups | $3,000 – $20,000/year |
These numbers shift based on factors affecting patient waitlist management software costs —such as region, developer expertise, integration complexity, and long-term support.
Want to get a more precise cost estimate for custom Patient Waitlist Management Software Development?
Discuss your project idea with our experts and get a tailored quotation.
Also Read: Cost of Custom Medical Billing Software
How to Choose the Right Development Partner
Picking the right technology partner for your patient waitlist management software project determines how well your system will perform, scale, and remain compliant in the years ahead.
The same holds for patient waitlist management software development- your partner must understand how clinical workflows, queue logic, and compliance frameworks connect to ensure the system truly works in practice.
Industry Experience That Actually Counts
Start with healthcare-specific experience. You need a team that has built EHR software, compliance-driven systems, and hospital waitlist system development projects before.
Partners who understand real-world hospital workflows will anticipate constraints rather than discover them mid-project. They’ll also know that HIPAA compliance isn’t a one-time checkbox but a design principle that influences every data-sharing decision.
A good partner brings knowledge of how trends of Patient waitlist management for hospital adoption are shaping global healthcare — from virtual queuing in outpatient departments to AI-assisted scheduling in multi-branch networks.
Customization Capabilities that Fit Your Operations
No two hospitals operate the same way. A qualified partner starts with discovery, learning how your clinicians, administrators, and IT teams actually function, before writing a single line of code. Effective developers build technology around your operations, not the other way around.
For example, one healthcare provider reduced nurse documentation time by 60% after switching to a vendor who customized the Patient scheduling and waitlist system for their exact shift rotation and staffing model.
This same adaptability applies to building Healthcare queue management software and integrating predictive analytics for load balancing.
Scalability for Long-Term Growth
Your system should grow as your organization expands. Ask potential partners how they plan to scale the patient waiting list management system modules across new facilities.
Microservices, API-first designs, and cloud infrastructures are essential for sustainable scalability.
Hospitals that invest in flexible foundations can easily extend their patient waitlist management software development when regulations or patient volumes change.
Support After Launch
The real test begins post-deployment. Healthcare environments evolve constantly—new rules, new security threats, new integration needs. Ask partners how they handle maintenance, patching, and upgrades. Do they proactively monitor systems or wait for incident reports?
Dependable vendors treat launch as the beginning of the relationship, not the end. Ongoing updates ensure the Digital Waitlist Management System remains compliant and efficient while supporting continuous performance improvements.
Red Flags Worth Noting
Be cautious of:
- Unrealistic timelines that ignore compliance review stages.
- Vague promises about “security” without outlining actual HIPAA measures.
- Thin healthcare portfolios with no previous patient waitlist management or EHR experience.
- A lack of curiosity- seasoned vendors ask tough questions early.
If a prospective partner can’t explain how they manage the patient waitlist management software development lifecycle or mitigate challenges in patient scheduling systems, consider it a warning sign.
Making Your Decision
Bring your clinical, administrative, and IT leaders into the evaluation process. Request detailed proposals demonstrating domain understanding, not just technical skill. Talk to previous clients with similar deployments. Strong references are the best validation of your vendor’s ability to deliver.
Ultimately, the right partner will combine deep healthcare experience with innovation, seamlessly aligning technology, compliance, and patient care.
Hospitals that align PMS projects with the use of Patient waitlist management software development initiatives tend to see faster adoption, stronger staff satisfaction, and measurable gains in operational efficiency.
Build Your Patient Waitlist Management System with Appinventiv
At Appinventiv, we don’t just build digital platforms; we design healthcare custom software development that improves how care is delivered. Our team of over 1,600 specialists has delivered 250+ healthcare projects globally, including advanced patient waitlist management software development, EHR/EMR platforms, and full hospital management systems.
We’ve helped hospitals:
- Reduce nurse response times by 60% with building Healthcare queue management software like YouCOMM.
- Connect 200+ medical devices through Health-e-People for personalized data insights.
- Improve diabetes care through connected wearables in DiabeticU.
Our services range from customized hospital waitlist systems to telemedicine apps, patient portals, and analytics dashboards, all compliant with HIPAA, GDPR, and local data-protection mandates.
If you’re looking to develop a waitlist management system for hospitals, integrate a Patient scheduling and waitlist system, or simply modernize your existing tech stack, we can guide you through every stage, from discovery to deployment and ongoing optimization.
Appinventiv ensures that your patient waitlist management initiatives evolve together, remain secure, are scalable, and are built to last. Connect with us today!
FAQs
Q. What is Patient Waitlist Management Software?
A. Patient waitlist management software is a digital tool that helps healthcare facilities organize, monitor, and reduce patient queues. Instead of relying on manual logs or phone calls, it automates adding patients to, prioritizing them on, and notifying them from the waitlist. Hospitals and clinics use it to balance appointments, handle cancellations in real time, and optimize staff schedules. For patients, it means less time waiting and more predictable care delivery.
Q. How Does AI Improve Patient Waitlist Management?
A. AI brings structure and foresight to a process that’s often unpredictable. Using real-time data — such as appointment history, treatment urgency, and patient behavior — AI models can forecast cancellations, identify bottlenecks, and automatically fill open slots.
For instance, if a patient cancels a visit, the system can instantly alert the next high-priority patient on the waitlist. AI also helps balance load across departments, ensuring no single provider or clinic gets overbooked. The result? Smoother patient flow, reduced idle time for staff, and higher patient satisfaction scores.
Q. How Can Healthcare Startups Digitize Patient Queues?
A. For healthcare startups, digitizing patient queues starts with replacing manual check-ins and physical waiting rooms with digital scheduling tools. Mobile apps or kiosks can let patients register remotely, view estimated wait times, and get live updates via SMS or push notifications.
Startups can also integrate queue management systems with EHRs or CRMs to automatically sync patient details. Adding simple automation — such as reminders or digital triage forms — reduces administrative overhead and speeds up consultations. The goal isn’t just efficiency, but also a more transparent, less stressful patient experience.
Q. How Long Does It Take to Build Patient Waitlist Software?
A. The development timeline depends on scope and complexity.
- A basic system with scheduling, alerts, and queue tracking typically takes 3 to 4 months to build.
- A more advanced solution that includes AI predictions, multi-clinic support, and EHR integration can take 6 to 9 months.
Timelines also vary based on the level of customization, regulatory compliance needs (like HIPAA or GDPR), and whether the solution is built from scratch or customized from an existing platform.
Q. Which Technologies Are Best for Healthcare Queue Management Apps?
A. Modern healthcare queue management apps rely on a mix of reliable and scalable technologies:
- Frontend: React.js or Angular for responsive user interfaces.
- Backend: Node.js, Django, or .NET Core for stable, secure logic.
- Database: PostgreSQL or MongoDB with encrypted data storage.
- Cloud: AWS or Azure for scalability and uptime.
- APIs & Integration: FHIR, HL7, and REST APIs to connect with EHRs, CRMs, and telehealth tools.
- AI Tools: TensorFlow or PyTorch for predictive modeling and demand forecasting.
This stack ensures the app remains secure, compliant, and adaptable as patient volumes grow.
Q. Why Is Patient Waitlist Management Important?
A. Because poor queue management affects more than just convenience — it affects care. Long, unmanaged waits can lead to delayed treatments, missed diagnoses, and patient drop-offs. For hospitals, it also means inefficient resource use and lower throughput.
An effective waitlist system streamlines scheduling, keeps patients informed, and helps clinicians focus on treatment rather than administrative work.
Q. What are the latest trends shaping patient waitlist management software?
A. Emerging technologies like AI scheduling, telemedicine integration, cloud infrastructure, blockchain security, and mobile accessibility are redefining how hospitals manage patient flow. These trends help reduce no-shows, improve scheduling efficiency, and create a more connected, patient-centric experience.
Q. What are the key benefits of using a patient waitlist management system?
A. A modern patient waitlist management system streamlines hospital operations by reducing administrative workload, improving scheduling accuracy, and enhancing patient experience through automated communication. It ensures data accuracy, supports HIPAA and GDPR compliance, provides actionable analytics, and scales easily as healthcare facilities grow—making it a vital tool for both operational efficiency and patient satisfaction.